🎧 Audio Version
If you have lived with PTSD, depression, anxiety, or ADHD, you have probably been told that your struggles are “all in your head.”
The truth is more intriguing and much more hopeful.
They are also in your gut.
The gut brain axis is the constant back-and-forth communication between your digestive system and your brain. It runs all day and all night, quietly shaping your mood, energy, stress response, and ability to focus. When the gut-brain axis is balanced, your mind feels steady, precise, and more resilient. Your nervous system can feel like it’s fighting you when it’s out of balance, no matter how hard you try to think.
In my work at MindLAB Neuroscience, I have spent more than twenty-five years watching how the gut-brain axis affects real people with real lives. I work with founders, traders, physicians, attorneys, creatives, and parents who are bright, responsible, and exhausted. Many have tried traditional talk approaches. They understand their story. They know their patterns. Despite this, their body still experiences unexpected jumps, collapses, or shutdowns.
This is where the gut-brain axis becomes a game-changer. When you know how your second brain works, and when you learn to train it in real time, you stop fighting your biology and start using it.

Listening To Your Second Brain: Why The Gut Brain Axis Matters Now
Most people think of the gut as a tube that deals with food. You eat, you digest, and you move on. The gut-brain axis tells a different story. Your gut is packed with nerve cells, neurotransmitters, and immune cells that talk directly to your brain. Some people call it the second brain.
That second brain continually sends signals through the vagus nerve, hormones, and immune messengers. Your brain listens. If the gut-brain axis is calm and well-regulated, the brain receives signals that convey safety, steadiness, and a sense of enoughness. When the gut-brain axis is inflamed, irritated, or out of rhythm, the brain hears danger, threat, or not enough, even when your thinking mind says everything is fine.
This explains why an individual suffering from PTSD may react violently when a door closes, despite being aware of their safety. It is why someone with depression can understand that their life is good on paper and still feel like they are wading through cement. This explains why a person suffering from anxiety may instruct themselves to calm down, despite their heart pounding. It is why someone with ADHD can swear they will slow down, then watch their body move before their brain has caught up.
In each of these cases, the gut brain axis is part of the story. It is not the only piece, but it is a powerful driver. When we ignore it, change feels almost impossible. When we target it with precision, change becomes not only possible but also sustainable.
How The Gut Brain Axis Actually Works In Your Body
To understand the gut-brain axis, picture a two-way highway between your gut and your brain.
One lane carries information up from your gut. This includes signals from the vagus nerve, which acts like a status report from your organs. It carries data about stretch, movement, and chemical signals. It also includes messages from your gut microbes, which create neurotransmitters like serotonin, dopamine, and GABA that affect how your brain fires.
The other lane carries information down from your brain. This includes your stress response. When your brain detects a threat, it sends signals that change how your gut moves, how much acid it makes, and how your immune cells behave. If this stress response stays high for too long, the gut lining can become more leaky, the microbiome can shift, and the gut-brain axis can fall into a new, less helpful pattern.

Over time, repeated stress, poor sleep, erratic eating, and unresolved trauma can train the gut-brain axis to expect danger. Once that pattern is wired in, your nervous system fires as if the worst were about to happen.
The key point is simple. The gut-brain axis learns. It is plastic. It can be rewired. That is where real-time neuroplasticity work comes in. When we ask the brain and gut to practice new patterns together, we are not trying to “think away” symptoms. We are retraining your entire system to react differently, starting from within.
The Gut Brain Axis And PTSD: When Survival Circuits Stay Stuck On
PTSD is not just about memories. It is about a body that has learned to live in a state of high alert.
For many of my clients with PTSD, the gut brain axis has been running in survival mode for years. Their gut is tight, their breathing is shallow, and their heart rate jumps at small sounds. They may have heartburn, irritable bowel symptoms, or cycles of nausea and loss of appetite. They often don’t link these patterns to their trauma, but the same nervous system loops cause both.
When the gut brain axis is traumatized, it tends to send frequent danger signals upward. The brain reads those signals as proof that the world is not safe. Thoughts follow the signals. This is why someone with PTSD can logically know they are not in danger, yet still feel as if they are back in the worst moment of their life.
Client Story: “Mark,” a combat veteran and executive
Mark is an anonymized client in his early forties. He served multiple tours and later became a senior executive. When he discovered MindLAB Neuroscience, he was successful at work yet miserable inside. He had nightmares, gut cramps, and sudden waves of rage that made him fear he would lose his career and his family. He had done talk-based work before. He could describe his trauma in detail, but his body still reacted as if he were under fire.
When we looked at his gut-brain axis, patterns jumped out. He skipped breakfast, drank coffee without eating, and went without food for many hours. Then he would overeat late at night. His gut was often bloated and painful. He lived in a constant state of internal tension.
We began with a simple experiment. Instead of talking first, we started by shifting the signals sent through his gut-brain axis. He practiced slow, paced breathing before meals, which stimulates the vagus nerve and tells the brain that the body is not in immediate danger. He added a consistent morning meal with protein and fiber so his gut wouldn’t go into panic mode by noon. During flashback spikes, instead of only analyzing his thoughts, he learned to notice the clench in his gut and use specific breath and posture cues to send different signals up the vagus nerve.
Over weeks, his gut pain eased. His startle response shrank. His nightmares have reduced. The past did not vanish, but his gut brain axis was no longer locked in permanent survival mode. His brain had new evidence that the war was over.
This is the power of pairing trauma work with the gut-brain axis. You are not telling yourself to get over it. You are showing your nervous system, step by step, that it is safe enough to stand down.
The Gut Brain Axis And Depression: When Life Feels Flat And Heavy
Depression is often described as sadness. Many of my clients do not feel sad. They feel nothing. They feel like their body has turned the volume down on life. Food has no taste, joy has no color, and even basic tasks feel like climbing a mountain.
The gut-brain axis plays a central role here. When this axis has been signaling threat or depletion for a long time, the brain sometimes responds by pulling back. It becomes more conservative with energy and reward. This can show up as low motivation, brain fog, and a sense that everything is too much.
On a gut level, clients with depression often describe constipation, sluggish digestion, or long-standing digestive discomfort. They may also have cravings for highly processed foods that give a quick dopamine hit but then cause a crash, which teaches the gut-brain axis to expect more ups and downs.
Client Story: “Sara,” tech leader who felt nothing
Sara is an anonymized client in her mid-thirties who led a high-performing product team. When she came to me, she described her life as “fine but blank.” Her relationships were stable, and her career looked impressive. Inside, she felt empty. She dragged herself through the day, then collapsed at night with her phone and junk food.
Her gut-brain axis was sending clear signals. She had frequent bloating, swings between constipation and diarrhea, and a sense of heaviness in her body. Mornings were the worst.
Rather than telling her to “think positive,” we approached the gut-brain axis as a target for real-time neuroplasticity. We built a gentle morning sequence that started before she even got out of bed. We established a brief breathing pattern that triggers the vagus nerve. She also drank a glass of water beside her bed. She followed a simple, repeatable breakfast routine that did not spike or crash her system.
During sessions, we mapped the moments when her energy dropped. We noticed that these often followed long stretches without food or movement. She practiced tiny movement breaks and brief “gut check” pauses, during which she placed a hand on her abdomen and noticed signals without judgment.
Week by week, her gut symptoms eased. Her energy rose. Her brain began to register more small hits of reward from daily life because her gut brain axis was no longer dragging her into shutdown. Her thoughts shifted after her physiology did. Not the other way around.
The Gut Brain Axis And Anxiety: When Your Body Will Not Stand Down
Anxiety is not just worry. It is a whole-body state, and the gut-brain axis is often at its center.
Clients with anxiety often describe a tight chest and a tight gut. They get “butterflies” that do not feel cute. Their stomach lurches before important meetings or social events. Some rush to the restroom. Others lose all appetite when they need energy most.
When the gut brain axis sends frequent, high-alert signals, the brain responds by scanning for danger. It then finds more reasons to worry, which sends more stress signals down to the gut. The loop becomes self-reinforcing.
Client Story: “Leah,” attorney with constant dread
Leah is an anonymized client in her early forties who worked in a fast-paced law firm. She described waking every morning with dread. Her stomach clenched before she even opened her eyes. By the time she got to the office, she had already run through every worst-case scenario in her mind.
When we explored her gut brain axis, we found a continuous stress pattern. She drank coffee immediately upon waking and often skipped food until late morning. Her gut was highly reactive. She had chronic reflux and constant tension in her abdomen. Her vagus nerve was essentially trained to signal “threat coming” every morning before her thinking brain had a chance to weigh in.
We began by using the gut-brain axis itself as a lever. Instead of scrolling through email in bed, she practiced a two-minute sequence of slow exhale breathing with one hand on her chest and one on her gut. This simple act begins to calm vagal firing. She delayed coffee until after she ate a small, simple breakfast. During the day, she set short “gut check” alarms to notice whether her abdomen was clenched. If it was, she stood, stretched, and took several slow breaths, which told her gut brain axis that she was not trapped.
These are not magic tricks. There are ways to use the gut-brain axis in real time. Over time, her morning dread loosened. She still had pressure at work, but her body no longer started the day at a ten out of ten on the anxiety scale. Her brain had more room to choose her response rather than react on autopilot.
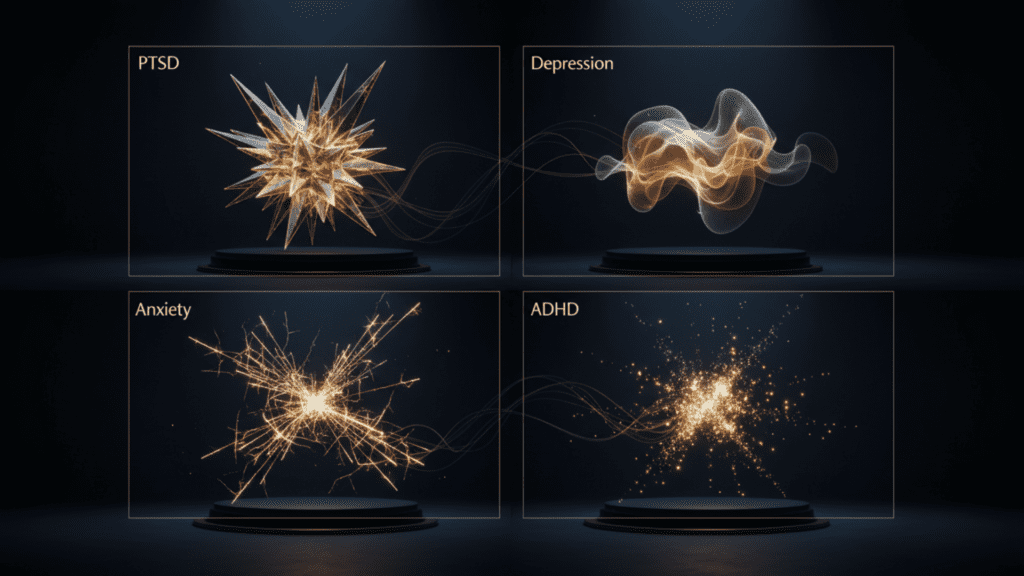
The Gut Brain Axis And ADHD: Focus, Impulse, And The Restless Brain
When people think about ADHD, they usually focus on attention and behavior. In my practice, I often see ADHD in the gut first.
Many clients with ADHD describe erratic eating. They go hours without eating, then binge. They crave fast carbs and sugar. They live on caffeine. Their gut brain axis learns that life is a series of feast-and-famine cycles. This pattern drives swings in dopamine and norepinephrine, making it even harder to focus.
The gut brain axis is closely linked to reward and motivation circuits. When the gut sends steady signals of safety and enough, the brain can invest energy in long-term tasks. When the gut brain axis says “now,” “urgent,” or “not enough,” the brain pushes you toward quick hits of stimulation. That might look like scrolling, impulsive decisions, or jumping between tasks.
Client Story: “Alex,” an Entrepreneur with ADHD
Alex is an anonymized client in his late twenties who built a successful startup. He described his mind as “hyper fast and scattered.” He could hyperfocus on a new idea, then crash and lose interest. He struggled to sit through meetings. He forgot to eat, then stuffed himself late at night.
We mapped his day through the lens of the gut brain axis. He realized that his sharpest crashes happened after long stretches without food, followed by big, heavy meals. His gut felt bloated and sluggish, and his brain followed.
Together, we built what I call a dopamine menu, including his gut. Instead of focusing solely on tasks, we looked at how the gut brain axis could send steadier signals. He practiced time-blocked eating windows, simple snack options that did not spike and crash his system, and micro breaks to monitor in with his breathing and gut tension.
He also learned to notice the early signs of a focus crash in his body, such as a hollow feeling in his stomach or a sudden sugar craving. Those were cues from his gut brain axis. Instead of judging himself, he used those cues to take a short reset. Over months, his focus stabilized. He still had an ADHD brain, but his gut brain axis was no longer throwing gasoline on every spark.
Neuroscience-Based Protocols To Reset Your Gut Brain Axis
Understanding the gut brain axis is only helpful if you can do something with it. This is where many people get stuck. They either try to overhaul everything at once or wait for motivation to appear. Neither works for long.
Real change comes from repeated, manageable actions that train the gut brain axis and the brain together. Here are the core principles I use inside MindLAB Neuroscience when I design protocols with clients who have PTSD, depression, anxiety, or ADHD.
First, we create safety signals on purpose. The gut brain axis closely monitors cues of safety and threat. Slow, extended exhales, gentle pressure on the abdomen, and rhythmic, comfortable movement all tell the vagus nerve that the body is not in immediate danger. When you pair these signals with moments that used to trigger you, you begin to teach the gut brain axis a new story.
Second, we stabilize basic rhythms. The gut brain axis loves pattern. Wild swings in sleep, food, and stimulus confuse it. You do not need a perfect routine, but you do need repeatable anchors. You should establish a consistent morning wake time, eat your first meal within a realistic timeframe, maintain regular movement, and implement a wind-down ritual that signals the end of the day to your system. Each of these anchors sends strong timing signals through the gut brain axis.
Third, we target specific symptom loops. PTSD might involve flashbacks, startle responses, and digestive spasms. Depression might bring heavy limbs, slow gut movement, and constant fatigue. Anxiety might heighten gut motility, cause cramps, or trigger nausea. ADHD might show up as erratic appetite and intense cravings. For each pattern, we design actions that leverage the gut brain axis.
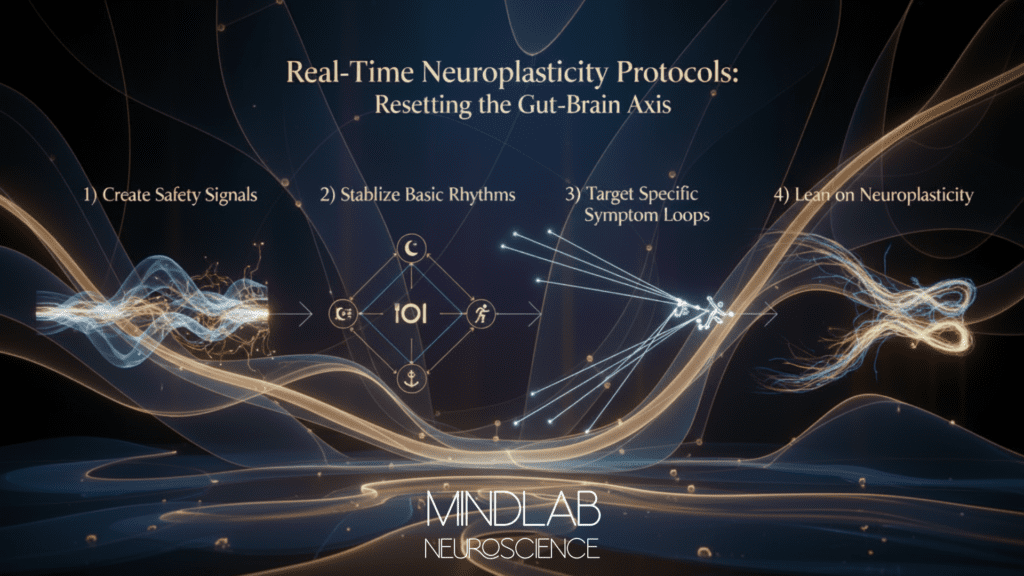
For example, a client with PTSD who freezes before speaking in public might practice a short gut and breath reset backstage. A client with depression who drifts into shutdown after lunch might pair that meal with a brief, enjoyable walk to give the gut brain axis movement data. A client with anxiety who dreads meetings might position their body in a way that frees the diaphragm and practice quiet belly breathing before logging on. A client with ADHD who jumps between tasks might use small, predictable snacks and short movement resets as cue points.
Fourth, we lean on neuroplasticity. The gut brain axis changes when you repeat new patterns while your nervous system is paying attention. That is why I focus on real-time neuroplasticity. We don’t just discuss your week; we also use what happens between sessions to train. When you feel your gut clench, that is a moment to practice a new response. You have the opportunity to choose a slightly different course of action when you recognize the urge to numb out.
Over weeks and months, these tiny choices add up. They carve new grooves in your gut brain axis. They change the way your brain predicts the world.
How I Use The Gut Brain Axis Inside MindLAB Neuroscience
My work is not traditional therapy. It is neuroscience-based coaching that considers your brain and body as a system that can learn. The gut brain axis is one of the core systems I map with every client.
In our first meetings, I listen for gut patterns. I ask about digestion, appetite, meal timing, and how your body feels when you struggle most. I combine those findings with what I know about PTSD, depression, anxiety, ADHD, and the way the gut brain axis shapes each one in slightly different ways.
Then we design experiments. I do not hand you a generic plan. Together, we build a set of small, precise changes. For one client, that might mean five minutes of a specific breathing pattern before bed to calm the gut brain axis overnight. For another, it might mean reshaping their entire morning so their gut and brain get clear signals that the day is starting with enough.
I also help clients make sense of what happens. When you know why your gut brain axis reacts the way it does, you feel less broken. You begin to see that your system is not failing; it is doing what it learned to do. That shift in meaning is decisive. It lets you move from shame to strategy.
Because I have spent decades inside the worlds of trauma, mood disorders, anxiety, ADHD, and high performance, I can help filter what actually matters. We ignore fads. We focus on what your brain and gut need in real time. We use concepts like dopamine, reward prediction, and neuroplasticity in a way that is simple enough to act on and deep enough to create lasting change.
Client Story: “Nina,” complex trauma, anxiety, and ADHD
Nina is an anonymized client in her late thirties with a history of complex trauma, chronic anxiety, and ADHD. She had tried multiple approaches before she came to MindLAB Neuroscience. She understood her past, but her days still swung between high anxiety, numbness, and frantic bursts of productivity.
Her gut brain axis was chaotic. She alternated between fasting all day when she was anxious and bingeing at night when she was exhausted. Her digestion was painful and unpredictable. Her constant fear of dropping one of the many balls she was juggling was ingrained.
We approached the gut brain axis as a central player. We began with a single non-negotiable anchor: a gentle, predictable first meal that she could tolerate even when she was anxious. We paired that meal with a short breathing and body scan sequence that calmed her vagus nerve and gave her a sense of agency.
Next, we worked on micro resets between tasks. Instead of racing from one demand to another, she practiced a twenty-second pause where she noticed her gut, relaxed her jaw, and stretched her chest. These small moves told the gut brain axis that she was not trapped and that she had choices.

Over time, we layered in more. We established a straightforward evening routine. We established a distinct bond with caffeine. We established more precise boundaries regarding the frequency of her phone checks. Each change was chosen because it affected the signals moving along the gut brain axis.
Months later, Nina described feeling “like my nervous system finally believes me when I say we are safe.” Her PTSD symptoms did not vanish, but her body was no longer living on red alert. Her depression lifts came less often and did not pull her as deeply. Her anxiety spikes came with more warning. Her ADHD brain still moved fast, but her gut brain axis was now an ally, not an enemy.
Bringing The Gut Brain Axis Into Your Daily Life
You might be wondering where to start. The gut brain axis can sound complex, yet the first steps are simple.
Begin by noticing your patterns without judgment. How does your gut feel in the morning, midday, and at night? When do your PTSD, depression, anxiety, or ADHD symptoms spike? What happens with your appetite and digestion in those windows?
Next, choose one place to practice. Maybe you start with your morning. Perhaps you start with how you handle conflict. Maybe you start by talking about how you recover after a tough day. In that chosen window, introduce a small action that sends a different signal through your gut brain axis. That could be a brief breathing pattern, a gentle meal, a short walk, or a simple body posture shift.
Then, repeat. The gut brain axis responds to repetition. You are teaching a new language.
As you do this, remember that setbacks are not proof that you are failing. They are part of the learning process. When your PTSD flares or your anxiety surges, when depression drags you down, or your ADHD pulls you off track, you can still use that moment. Notice your gut and practice a small signal that tells your nervous system, “I hear you, and we are not in the same danger anymore.”

Bringing It All Together: Restoring Your Gut Brain Axis And Your Life
The gut brain axis is not a trend. It is a core part of how your nervous system stays alive, learns, and changes. When you understand it, you gain a powerful lever for reshaping PTSD patterns, lifting depression, calming anxiety, and stabilizing ADHD.
Your second brain is not working against you on purpose. It has been trained by years of experience, many of which were outside your control. The gut brain axis did what it had to do to keep you alive, even if that now shows up as pain, tension, or numbness.
The hope is this. What has been trained can be retrained. Your gut brain axis is plastic. With the right kind of attention and repetition, it can learn new patterns.
In my work at MindLAB Neuroscience, I have watched clients who felt broken begin to trust their own bodies again. I have seen people with brutal trauma histories feel safe enough to sleep. I have watched clients with deep depression feel small sparks of joy again. I have helped anxious and ADHD brains find a new rhythm that lets them perform at a high level without burning out. In each case, the gut-brain axis was part of the path.
You do not have to fix everything today. You do not have to earn the right to feel better. You do not have to choose between your brain and your body. You can start by listening differently to the signals coming from your gut. You can begin by sending just one new signal back.
From there, step by step, breath by breath, meal by meal, you can retrain your gut-brain axis and your life at the same time.
Questions I am Asked Most Frequently
How does Real-Time Neuroplasticity help retrain your gut brain axis at MindLAB Neuroscience?
Real-Time Neuroplasticity means we work with your brain and gut while life is actually happening, not only in a session. I help you notice when your gut-brain axis goes into old patterns, like clenching, shutting down, or racing. In those exact moments, you practice simple, science-based resets like specific breathing, posture changes, and the timing of food that send new signals up the vagus nerve. u003cbru003eu003cbru003eOver time, these repeated “in the moment” reps teach your gut brain axis that it does not have to react with the same level of danger. You are not just learning ideas; you are training a new default setting in your nervous system.
What makes MindLAB Neuroscience different from traditional talk-based approaches for PTSD, depression, anxiety, and ADHD?
At MindLAB Neuroscience, I start with your brain and body as a single system, not just your thoughts. I map how PTSD, depression, anxiety, or ADHD show up in your gut brain axis, sleep, and stress response. Instead of asking you to discuss the same story for years, I design precise, real-time experiments that test how your system responds when we change signals through the gut and the brain together. You get clear, practical tools that fit your real life, backed by more than twenty-five years of clinical neuroscience experience. The goal is not insight alone; the goal is measurable change in how you feel and function.u003cbru003e
How do you actually work with the gut brain axis inside a session?
In our work together, I ask specific questions about your digestion, appetite, energy crashes, and gut tension across the day. We tie those gut patterns to the moments your PTSD, depression, anxiety, or ADHD symptoms spike. Then I help you build small, targeted moves, such as how you breathe before a meeting, what you eat first thing in the morning, or how you reset your body after a conflict. u003cbru003eu003cbru003eWe track how your gut brain axis responds over days and weeks, then adjust the plan based on data, not guesswork. You leave each session with clear next steps, not vague advice.
Can my brain and gut still change if I have tried many other things and nothing has lasted?
Yes, they can. Your gut brain axis and your brain remain plastic throughout your life, meaning they can still learn new patterns. Many of my clients come to MindLAB Neuroscience after years of trying other methods and feeling broken or hopeless. u003cbru003eu003cbru003eOnce we address their symptoms as learned survival strategies and include the gut-brain axis in the plan, change starts to feel possible again. We build tiny, repeatable wins that your nervous system can trust, instead of swinging between extreme plans and crash cycles. Over time, this steady, neuroscience-based approach produces fundamental, lasting shifts.u003cbru003e
What does the first month with MindLAB Neuroscience usually look like for someone struggling with gut-brain axis issues and mental health symptoms?
In the first 30 days, we focus on mapping and stabilizing. I get a detailed picture of your history, your current symptoms, and how your gut brain axis behaves across a typical week. u003cbru003eu003cbru003eTogether, we choose a few high-impact targets, like your mornings, your sleep, or your pre-stress routine, and we design Real-Time Neuroplasticity exercises around them. You will test these strategies in your daily life, and then we will review what worked, what did not, and why, using brain and body science rather than assigning blame. By the end of that first month, you usually clearly understand your own gut-brain axis, a set of tools that fit your life, and early proof that your system can, in fact, change.