🎧 Audio Version
When someone experiences suicidal thoughts, it’s not simply a matter of willpower, choice, or character. The neuroscience of suicidal ideation reveals that these overwhelming thoughts emerge from complex, measurable changes in brain structure, chemistry, and function. Understanding this science doesn’t diminish the emotional pain people feel; instead, it illuminates why crisis feels so consuming and, most importantly, why recovery is genuinely possible. The brain is remarkably adaptable, and while specific neurobiological patterns contribute to suicidal thinking, this same neuroplasticity offers profound hope for wellness and recovery.
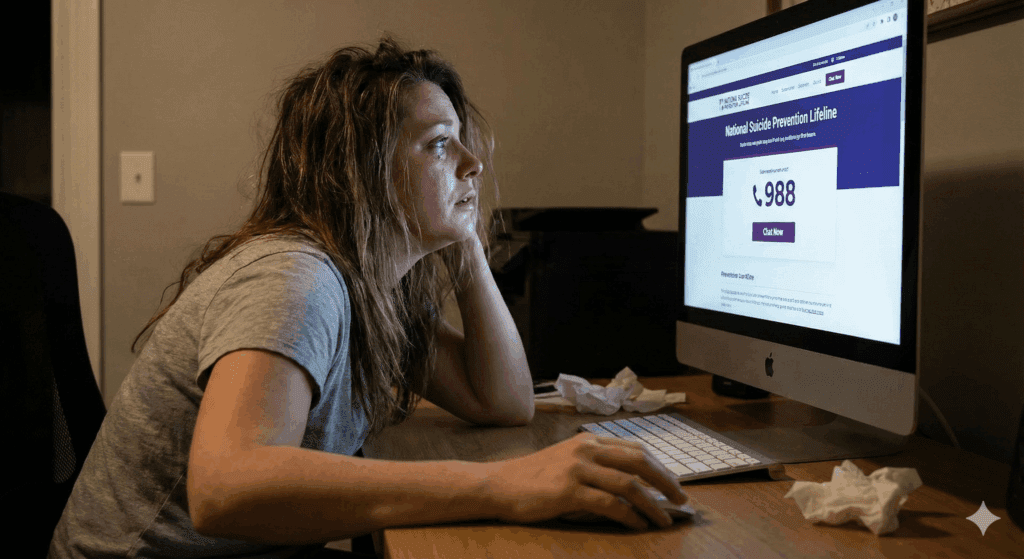
If you’re reading this because you or someone you love is struggling, please know that what you’re experiencing has biological underpinnings that can be understood, addressed, and resolved. The neuroscience of suicidal ideation shows us that the brain can change, thoughts can shift, and hope can be restored. You’re not broken; your brain is responding to stress, trauma, or chemical imbalances in predictable ways, and there are pathways back to wellness.

How the Brain Creates a Crisis
The neuroscience begins with understanding how the brain processes emotions, makes decisions, and responds to stress. Multiple brain regions work together in an intricate network, and when this network becomes dysregulated, suicidal thoughts can emerge. The prefrontal cortex, particularly the frontal pole and the dorsolateral prefrontal cortex, plays a central role in decision-making, problem-solving, and impulse regulation. Research shows that individuals experiencing suicidal thoughts often have altered structure and function in these regions. Suicidal ideation refers to recurring thoughts, wishes, or plans about suicide that emerge from specific patterns of brain dysregulation rather than character weakness or intentional choice.
Studies examining the neuroscience of suicidal ideation have found that young people who have attempted suicide demonstrate reduced surface area in the frontal pole, suggesting this structural difference may represent a vulnerability factor. When these frontal regions aren’t functioning optimally, it compromises our ability to think through problems, envision future possibilities, and inhibit harmful impulses. It’s like trying to navigate through fog: the path forward becomes unclear, alternatives seem invisible, and dangerous options may appear to be the only way out.
The ventromedial prefrontal cortex, another critical area, helps us assign value to different choices and outcomes. The neuroscience of suicidal ideation reveals that this region often shows disrupted activity in people who have made suicide attempts, making it difficult to weigh the consequences of decisions accurately. When someone is in crisis, this impaired value processing can make suicide seem like a reasonable solution rather than the permanent tragedy it truly is. The brain’s capacity to accurately assess risks and benefits is fundamentally changed.
The Emotional Brain and the Weight of Pain
The neuroscience of suicidal ideation also involves limbic structures that govern our deepest emotions. The amygdala, often called the brain’s alarm system, processes threats and emotional responses. Studies indicate that individuals with suicidal thoughts frequently exhibit heightened amygdala activity, especially when confronting negative stimuli. This hyperactivation intensifies feelings of fear, anxiety, and emotional pain, creating a feedback loop that reinforces hopelessness. Imagine an alarm system that won’t turn off, constantly signaling danger even when you’re safe. That’s what many people experiencing suicidal thoughts endure neurologically.
The anterior cingulate cortex bridges emotional and cognitive processing, acting as a critical integration point. The neuroscience of suicidal ideation demonstrates that this region shows altered connectivity in people experiencing suicidal thoughts, affecting their ability to regulate emotional responses and suppress negative self-thinking. When viewing emotionally expressive faces, suicide attempters show greater activation in the anterior cingulate cortex compared to those without a suicide history, indicating different processing of emotional stimuli. This heightened reactivity means that social interactions and others’ emotional expressions can feel overwhelmingly intense.
Research on the neuroscience of suicidal ideation in adolescents reveals that glutamatergic metabolism in the anterior cingulate cortex differs significantly between depressed youth with and without suicidal ideation. Specifically, those experiencing suicidal thoughts show alterations in glutamate and related compounds, neurotransmitters essential for learning, memory, and emotional regulation. These changes affect how the brain processes emotional salience, making negative experiences feel more significant and positive experiences less impactful.
The hippocampus, essential for memory formation and stress regulation, often shows reduced volume in individuals with depression and suicidal thoughts. This reduction, linked to chronic stress and elevated cortisol levels, impairs the ability to process current information contextually and contributes to feelings of hopelessness. The neuroscience of suicidal ideation reveals that these hippocampal changes affect how people remember their past and imagine their future, making it harder to envision hope or recall moments of joy. When your memory systems are compromised, it becomes difficult to remember that you’ve survived hard times before or to imagine that things could improve.

The Chemistry of Crisis
The neuroscience of suicidal ideation extends beyond brain structure to the chemical messengers that neurons use to communicate. Serotonin, the neurotransmitter most associated with mood regulation, consistently shows altered function in individuals with suicidal thoughts. Research on cerebrospinal fluid indicates that individuals with serotonin metabolite levels below the median are considerably more prone to suicide. This serotonin depletion affects mood, sleep, appetite, and the ability to experience pleasure, creating a biological foundation for despair.
When serotonin levels drop, the neuroscience of suicidal ideation shows that the brain loses its natural buffer against negative emotions. It’s like removing shock absorbers from a car; every bump in the road feels jarring and overwhelming. Small setbacks feel catastrophic, minor criticisms feel devastating, and the emotional pain becomes physically unbearable. Risk factors for suicidal ideation include neurochemical imbalances in serotonin and GABA, inflammation markers in the brain, altered stress response patterns, and structural white matter disruptions that together create biological vulnerability.
Dopamine, involved in motivation, reward, and pleasure pathways, also plays a role in the neuroscience of suicidal ideation. Disruptions in dopamine functioning contribute to feelings of hopelessness and the inability to experience joy, a condition called anhedonia. When the brain’s reward system isn’t working correctly, activities that once brought satisfaction feel meaningless, and life itself can seem devoid of purpose. The neuroscience of suicidal ideation reveals that the cause isn’t about lacking gratitude or being ungrateful; it’s about a biological system that has stopped responding to positive stimuli.
GABA, the brain’s primary inhibitory neurotransmitter, helps maintain emotional stability and calm neural activity. The neuroscience of suicidal ideation shows that reduced GABA levels are strongly associated with suicidal behavior. Research demonstrates that serum GABA concentrations are significantly lower in clients with depression who exhibit suicidal behavior compared to those without suicidal thoughts. This GABA depletion creates an imbalance between excitation and inhibition in the brain, making it harder to regulate emotions and suppress harmful impulses.
Think of GABA as the brain’s brake system. The neuroscience of suicidal ideation indicates that when GABA function is impaired, the brain loses its ability to slow down racing thoughts, calm intense emotions, and prevent impulsive actions. Everything feels accelerated and out of control, making it nearly impossible to attain peace or think clearly.
Glutamate, the brain’s primary excitatory neurotransmitter, also factors into the neuroscience of suicidal ideation. Elevated glutamate activity, particularly when combined with reduced GABA function, can lead to excitotoxicity, literally overwhelming and damaging brain cells. This imbalance contributes to the intense, racing thoughts and emotional turbulence characteristic of suicidal crises. The neuroscience of suicidal ideation indicates that this excitatory/inhibitory imbalance induces a neurological condition in which the brain is unable to achieve equilibrium.
When Inflammation Invades the Brain
Recent discoveries in the neuroscience of suicidal ideation highlight the role of neuroinflammation, a finding that has transformed our understanding of suicide risk. Studies examining postmortem brain tissue from suicide victims consistently find elevated markers of inflammation, including increased levels of interleukin 6 and other cytokines. This inflammation appears to be more than a coincidence; it actively contributes to suicidal risk.
Neuroscience shows that neuroinflammation makes microglia, which are the brain’s immune cells, more active. When overactivated, these cells release inflammatory chemicals that disrupt normal brain function, interfere with neurotransmitter production, and damage neural connections. Research shows that cerebrospinal fluid from suicide attempters contains significantly elevated levels of quinolinic acid, an inflammatory metabolite that can reach levels 300 percent higher than usual. This compound promotes inflammation and depletes serotonin, creating a vicious cycle.
Understanding the neuroscience of suicidal ideation through the lens of inflammation helps explain why physical health problems, chronic pain, and autoimmune conditions increase suicide risk. When the body is inflamed, the brain becomes inflamed too, and this neuroinflammation directly affects mood, cognition, and impulse control. It’s not just that chronic illness causes depression; the inflammation itself changes brain chemistry in ways that promote suicidal thinking.
The neuroscience of suicidal ideation also connects inflammation to daily stress responses. Studies using brain imaging indicate that individuals with elevated markers of neuroinflammation experience more severe suicidal thoughts when exposed to everyday stressors. This suggests that inflammation may sensitize the brain, making people more vulnerable to suicidal thinking during challenging moments. It’s like having an immune system in the brain that overreacts to threats, turning manageable stress into an unbearable crisis.
The Stress Response System Under Siege
The hypothalamic-pituitary-adrenal axis governs how the body responds to stress, and its dysregulation is central to the neuroscience of suicidal ideation. When functioning correctly, this system helps us adapt to challenges by releasing cortisol and other stress hormones in appropriate amounts. However, chronic stress can dysregulate this axis in ways that increase suicide risk.
Interestingly, the neuroscience of suicidal ideation reveals a paradox that surprised researchers. While depression often involves hyperactive stress responses, individuals who attempt suicide frequently show blunted cortisol reactivity. This blunted response means that when faced with stressors, their bodies don’t mount an adequate physiological response to mobilize coping resources.
Research demonstrates that adolescents with blunted cortisol responses are significantly more likely to attempt suicide when experiencing peer stress. In contrast, those with normal stress responses experience only suicidal thoughts without progressing to attempts.
The neuroscience of suicidal ideation suggests that this blunted stress response impairs adaptive coping mechanisms. When the brain cannot properly mobilize resources to meet challenges, manageable problems feel insurmountable, minor setbacks seem catastrophic, and the future appears hopeless. This biological vulnerability, combined with environmental stressors, creates conditions where suicide seems like the only escape from unbearable circumstances.
Brain Connectivity and Communication Breakdown
The neuroscience of suicidal ideation also examines how different brain regions communicate through white matter tracts, the nerve fiber highways connecting distant brain areas. Disruptions in white matter integrity appear consistently in people who have attempted suicide. Studies using advanced brain imaging find reduced structural integrity in white matter tracts connecting frontal and limbic regions in suicide attempters.
Specifically, the neuroscience of suicidal ideation identifies disruptions in the inferior fronto-occipital fasciculus, superior longitudinal fasciculus, and corpus callosum, pathways critical for integrating cognitive control with emotional processing. These disruptions make it harder for the brain to coordinate responses, which leads to bad decisions and trouble controlling emotions. It’s like having phone lines cut between different departments in an organization; the logical thinking center can’t effectively communicate with the emotional processing center, leading to disorganized responses to stress.
Research on white matter hyperintensities reveals that individuals with mood disorders who have these brain lesions are more than twice as likely to have attempted suicide. The neuroscience of suicidal ideation indicates that these structural alterations, whether preexisting vulnerabilities or results of chronic stress and inflammation, fundamentally change how the brain processes information during crisis.

When Neuroplasticity Falters
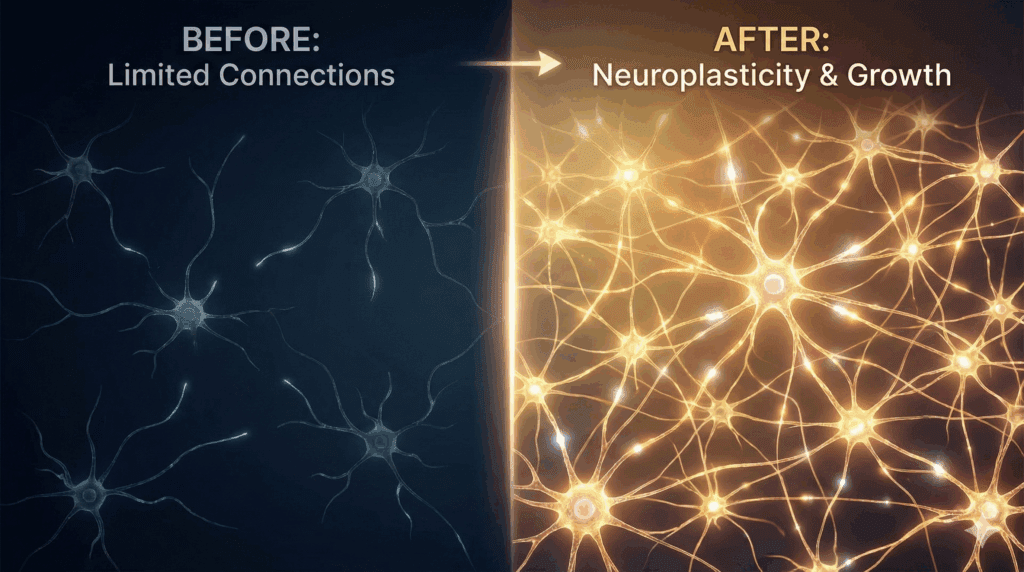
The neuroscience of suicidal ideation reveals critical changes in neuroplasticity, the brain’s ability to form new connections and adapt to experiences. Brain-derived neurotrophic factor, a protein essential for neuroplasticity, shows consistently reduced levels in individuals with suicidal thoughts. Research on postmortem brain tissue indicates diminished BDNF expression in the prefrontal cortex and hippocampus of suicide victims, with certain studies revealing hypermethylation of BDNF genes that inhibit its synthesis.
This reduction in BDNF profoundly affects the neuroscience of suicidal ideation by impairing the brain’s ability to adapt to stress and form new neural pathways. When neuroplasticity is compromised, people become stuck in rigid thought patterns, lose the flexibility needed to envision alternatives, and can’t create new memories that contradict their hopeless narratives. The brain essentially becomes locked into patterns of despair, unable to rewire itself toward hope.
However, this aspect of the neuroscience of suicidal ideation also offers tremendous hope. Because BDNF levels can be restored through interventions like exercise, therapy, medication, and mindfulness practices, the brain’s capacity for change can be reawakened. When BDNF increases, new neural pathways form, rigid thinking patterns loosen, and the capacity to experience hope and imagine alternatives returns. Neuroplasticity works both ways; just as the brain can change in directions that promote suffering, it can also change in directions that restore wellness.
Decision Making Under Duress
The neuroscience of suicidal ideation illuminates how cognitive control breaks down during crisis, helping us understand why people who usually are thoughtful and careful can make tragic, impulsive decisions. Decision-making studies reveal that suicide attempters show impaired performance on tasks requiring value-based choices, particularly when emotional feedback is involved. Functional brain imaging during decision-making tasks shows that individuals with a suicide history display altered activation patterns in the orbitofrontal cortex and dorsolateral prefrontal cortex.
The neuroscience of suicidal ideation demonstrates that these decision-making impairments aren’t simply about impulsivity in the traditional sense. Research identifies distinct neural mechanisms: some individuals show neglect of decision-relevant information, with blunted value signals in the ventromedial prefrontal cortex, while others exhibit increased delay discounting, with altered basal ganglia function. Both patterns make suicide seem like a viable option rather than the devastating loss it represents.
Understanding the neuroscience of suicidal ideation helps explain why people in crisis can’t “just think it through” or “see reason.” Their decision-making neurocircuitry is fundamentally altered, making it neurologically difficult to accurately weigh options, consider consequences, or imagine future scenarios. It’s not a character flaw; it’s a brain state that requires intervention and support to restore normal functioning.
Suicidal attempters disrupt the normal relationship between impulsivity and prefrontal frontoparietal connectivity, as revealed by the neuroscience of suicidal ideation. This disconnection means that even when cognitive control systems attempt to inhibit harmful actions, the signals fail to translate into behavioral inhibition. The brake pedal is pressed, but the brake line has been severed.

The Kynurenine Pathway Connection
The neuroscience of suicidal ideation has uncovered the kynurenine pathway as a crucial mechanism linking inflammation, neurotransmitter depletion, and brain toxicity. When inflammation activates this metabolic pathway, it diverts tryptophan away from serotonin production and instead produces compounds such as quinolinic acid. This cycle creates a triple burden: depleted serotonin reduces mood stabilization, elevated quinolinic acid promotes excitotoxicity and further inflammation, and the inflammatory process perpetuates itself.
Studies on cerebrospinal fluid reveal significant correlations among quinolinic acid levels, interleukin 6 concentrations, and the severity of suicidal ideation scores. The neuroscience of suicidal ideation suggests this pathway represents a targetable mechanism for intervention, potentially explaining why anti-inflammatory approaches show promise in reducing suicide risk. This discovery offers hope because interventions that reduce systemic inflammation, from dietary changes to anti-inflammatory medications to stress reduction techniques, may help restore healthier brain chemistry.
Age Differences in Vulnerable Brains
The neuroscience of suicidal ideation varies across the lifespan, with adolescent and young adult brains showing different patterns than adult brains. Young people’s brains are still developing, particularly the frontal limbic systems responsible for emotional regulation and impulse control. Studies comparing adolescent and adult suicide attempters indicate that structural brain alterations may be subtler in youth but are still significant and predictive of risk.
Research on the neuroscience of suicidal ideation in children reveals particularly concerning findings. An extensive study of children aged 9 to 11 found that approximately 8 percent had experienced suicidal thoughts or behaviors, with brain connectivity patterns that differed from healthy peers. The neuroscience of suicidal ideation in this young population shows disruptions in connector hubs, brain regions that link different networks together, particularly in girls who progressed from ideation to attempt.
Understanding the neuroscience of suicidal ideation across development helps explain why adolescence represents such a vulnerable period. The prefrontal cortex, which provides executive control and impulse inhibition, doesn’t fully mature until the mid-twenties, while the limbic system, responsible for emotional intensity, is highly active during adolescence. This creates a developmental window in which emotional storms are intense, but the braking mechanisms are still under construction; intervention and support are especially critical during these years.

How Suicidal Ideation Differs from Depression
While depression and suicidal thinking often co-occur, the neuroscience of suicidal ideation demonstrates they have distinct biological underpinnings that require specific attention. Research comparing depressed individuals with and without suicidal thoughts finds specific differences; those with suicidal ideation show greater reductions in frontal pole surface area, more pronounced white matter disruptions, and different patterns of amygdala connectivity. Types of suicidal ideation range from passive wishes to die, to active planning with specific intent, each representing different levels of neurobiology dysregulation that benefit from targeted neuroscience-based intervention.
The neuroscience of such ideation reveals that suicidal behavior represents a specific psychopathological process beyond depression symptoms alone. Research indicates that alterations in brain regions such as the anterior insula correlate with suicide risk, irrespective of the severity of depression. This distinction carries profound clinical implications because it means sessions must address suicide risk directly rather than assuming depression treatment alone will eliminate suicidal thoughts.
Understanding the neuroscience of suicidal ideation as distinct from depression helps explain why some people with severe depression never experience suicidal thoughts. In contrast, others with seemingly milder depression may be at high risk. The particular combination of brain alterations, neurotransmitter dysregulations, inflammatory indicators, and genetic influences engenders a susceptibility to suicide that transcends mere mood symptoms.
How the Neuroscience of Suicidal Ideation Informs Personalized Coaching
The most important message from the neuroscience of suicidal ideation is this: if the brain can change in directions that create vulnerability and crisis, it can also change in directions that restore health and hope. Neuroplasticity can trap someone in patterns of despair, but it can also free them when the right interventions are applied. Every discovery about how the brain creates this ideation simultaneously reveals potential targets for restoration.
Neuroscience-based coaching specifically designed for suicide prevention has shown remarkable effectiveness and helps explain why. These approaches directly target the cognitive rigidity and emotion dysregulation that characterize suicidal states by working with the brain’s capacity for change rather than against it. Unlike traditional talk therapy or random crisis lines, neuroscience-based coaching applies understanding of neuroplasticity to create measurable shifts in how the brain processes threat, meaning, and possibility.
At the core of neuroscience-based coaching is thought reframing informed by how the brain actually works. When someone is experiencing suicidal ideation, their prefrontal cortex, the brain’s rational planning center, has been hijacked by hyperactive limbic regions screaming danger signals. Neuroscience shows that standard cognitive interventions often fail because they try to reason with a brain that is physiologically incapable of reasoning in that moment. Neuroscience-based coaching instead uses understanding of these mechanisms to create interventions that work with the brain’s current state rather than against it.
Thought reframing in neuroscience-based coaching means helping your brain recognize that suicidal thoughts are outputs of a dysregulated system, not truth about your life or your future. When your amygdala is hyperactivated and your prefrontal cortex is offline, the thoughts feel absolutely real and entirely true. Neuroscience-based coaching teaches you to recognize this perception as a brain state, not reality.
You learn to observe thoughts like “I should die” or “Everyone would be better off without me” as symptoms of your brain’s current dysregulation, similar to how someone with a fever has ideas that feel real but reflect their elevated temperature rather than truth.
The neuroscience demonstrates that this type of thought observation activates your prefrontal cortex, literally bringing your rational brain back online even during a crisis. By naming what’s happening neurobiologically, you create psychological distance from suicidal ideation. You’re no longer fused with the thought; you’re observing it as a symptom. This subtle but profound shift in perspective corresponds to measurable changes in brain activation patterns, particularly in regions responsible for self-referential thinking and emotional regulation.
Fixing distorted thoughts using neuroscience is more effective than regular cognitive therapy because it targets the brain processes that cause these distortions right from the start. Suicidal ideation creates predictable patterns of thinking: catastrophizing, where you imagine the worst possible outcome and assume it will happen; overgeneralization, where one setback feels like confirmation of permanent failure; mental filtering, where you ignore all positive evidence and focus only on negative; and personalization, where you assume responsibility for things beyond your control.
The neuroscience shows that these aren’t character flaws or logical errors you should be able to think away; they’re outputs of an amygdala that is flooding your system with threat signals while your prefrontal cortex lacks the resources to provide accurate perspective.

When working with a neuroscience-based coach who knows you, understands your specific brain vulnerabilities, and has access to you 24/7, the correction of these distortions becomes personalized and timely. Instead of waiting days for an appointment or calling a suicide line where you explain your situation to a stranger who doesn’t know your history, a doctor who knows you can recognize distorted thinking patterns the moment they emerge. Your coach knows that when you start talking about being a burden, your particular brain is running a specific distortion pattern that, in your case, often precedes crisis. They can intervene at that moment with approaches specifically tailored to how your brain responds.
The difference between calling a random suicide prevention line and having 24/7 access to a doctor who knows you and is genuinely invested in your life represents a paradigm shift in suicide prevention. When you’re in crisis and call an anonymous crisis line, several neurobiological barriers exist. First, your prefrontal cortex is already compromised, making it difficult to explain what’s happening coherently. Second, the person on the line doesn’t know your history, your triggers, or what approaches work for your particular brain. Third, there’s no continuity; you might speak with a different person each time, meaning you start from zero each call.
The neuroscience of suicidal ideation reveals why continuity and relationship matter neurologically. When you’re in crisis, your brain is flooded with cortisol and adrenaline. Your amygdala is screaming danger. Your threat detection systems are maxed out. Currently, your brain needs safety signals. Neurobiologically, safety signals come from connections with someone your brain has learned to trust, someone whose presence and voice calm your nervous system. A neuroscience-based coach you’ve worked with intensively becomes what’s called a “co-regulator.” Your brain has learned through repeated positive interactions that this person represents safety. When you connect with them during a crisis, your nervous system begins to calm simply from that connection.
Research shows that this nervous system co-regulation literally changes brain state. When you hear the voice of someone your brain recognizes as safe, your amygdala shows reduced activation. Your HPA axis stress response begins to normalize. Your prefrontal cortex regains some capacity for rational thought. None of this happens when you call a stranger, no matter how skilled that stranger is, because your brain hasn’t learned to recognize them as a safety signal.
Having 24/7 access to your neuroscience-based coach means interventions can happen in the moment. The neuroscience of suicidal ideation shows that suicidal crises often pass within hours if someone receives appropriate support during those critical hours. If you have to wait days for an appointment or if you’re relying on crisis lines, you’re trying to weather the storm alone. With 24/7 access to your doctor, you can reach out when the storm is building. Your coach can help you apply neuroscience-based interventions before a crisis fully develops.
At the moment when cognitive distortions are forming, when your brain is beginning to believe the lies that suicidal ideation generates, your coach can intervene. They know your specific pattern. They know that before you think, “I should die,” you typically have thoughts about being a burden or not mattering. They can catch you at the distortion stage, before it spirals into active suicidal planning. They can remind you neurobiologically what’s happening: that your amygdala is in overdrive, that your threat detection is too sensitive, and that the thoughts feel true but don’t reflect reality.
This type of therapy is the game changer. It’s not that neuroscience-based coaching is fundamentally different from other approaches in its techniques. It’s that having continuous access to someone who knows your brain, understands your neurobiology, and can intervene throughout your life rather than during scheduled appointments means that suicidal crises can be caught, turned around, and prevented from escalating to the point of attempts. The neuroscience of suicidal ideation demonstrates that most people in suicidal crisis experience warning signs over hours or days. With 24/7 access to a neuroscience-based coach invested in your life, those warning signs can be caught and addressed in real time.
Beyond crisis intervention, continuous access to neuroscience-based coaching facilitates neuroplasticity in ways that periodic therapy cannot. Neuroplasticity requires repeated activation of new neural pathways. Every time you catch a distorted thought and reframe it neuroscientifically, every time you notice your amygdala overreacting and consciously engage your prefrontal cortex, and every time you name what’s happening in your brain rather than identifying with it, you’re strengthening new pathways and weakening old ones. With periodic therapy appointments, this neural rewiring happens between sessions. With 24/7 access to a coach, the rewiring can happen continuously.
Think of neuroplasticity like building a new neural highway. Each time you use the new pathway, you strengthen it. With traditional therapy once weekly, you’re working on your new highway one hour per week. With 24/7 access to a neuroscience-based coach, you’re reinforcing that new pathway every single day, multiple times per day when needed. Over months and years, this continuous reinforcement creates profound changes in how your brain functions. Neural pathways associated with suicidal thinking literally weaken from disuse, while new pathways associated with hope, resilience, and meaning grow stronger and more accessible.
Neuroscience-based coaching utilizes neuroplasticity intentionally and strategically. Your coach doesn’t just teach you information about how your brain works; they guide you to use that knowledge to actively reshape your neural architecture. When you understand that your suicidal thoughts emerge from a specific brain state created by specific neurotransmitter imbalances, inflammatory processes, and stress response dysregulation, you stop blaming yourself for having them. This shift alone produces neuroplastic change; the brain regions responsible for self-criticism and shame become less active, while areas associated with self-compassion activate more strongly.
Your neuroscience-based coach helps you recognize that every intervention you pursue, from exercise to sleep optimization to stress reduction to social connection, isn’t just making you feel better; it’s literally changing your brain at the structural and chemical level. This knowledge itself becomes motivating neurobiologically. When you understand that a walk in nature doesn’t just distract you but actually increases BDNF production and reduces inflammation in your brain, you’re more likely to take it. When you understand that reaching out to a friend doesn’t just make you feel less lonely but actually normalizes your stress response systems, you’re more likely to make that connection. The neuroscience of suicidal ideation becomes empowering knowledge that fuels the very behaviors that create wellness.
The combination of neuroscience-based coaching with 24/7 access represents a fundamental shift in how suicide prevention can work. Instead of hoping people in crisis reach out to anonymous services, you have a continuous relationship with someone invested in your specific brain, your specific vulnerabilities, and your specific path back to wellness. Instead of relying on coping skills you learned in therapy appointments, you have real-time guidance from someone who knows exactly how your brain responds to interventions. Instead of trying to think your way out of suicidal ideation using willpower alone, you have neurobiological support for the brain changes that create a lasting shift away from suicidal thinking.
This is why access to your neuroscience-based doctor 24/7 becomes the game changer. You’re not calling a random suicide line where someone who doesn’t know you tries to help. You’re connecting with a doctor who knows your neurobiology intimately, who has studied your specific pattern of brain dysregulation, and who is genuinely invested in your life and recovery. That doctor can recognize the subtle signs that your brain is moving into crisis territory.
Before you get to the stage of actively planning your suicide, they can step in. They can guide you to use your understanding of your own neuroplasticity to actively rewire your brain away from patterns of despair and toward patterns of hope. And most importantly, they’re accessible in the moments when you need them most, making the difference between weathering a crisis and losing a life. In neuroscience-based coaching, assessing suicidal thoughts looks at more than just symptoms; it examines your unique brain issues, signs of brain inflammation, how your body responds to stress, and any thinking errors related to your brain’s biology

Connection as Medicine
Perhaps one of the most powerful findings from research on the neuroscience of suicidal ideation is how profoundly social connection affects brain function and suicide risk. Studies show that perceived social support reduces suicide risk by 40 to 47 percent, with effects on suicidal ideation, suicide plans, attempts, and deaths. This isn’t just about feeling less alone; social connection produces measurable changes in brain chemistry and function.
The neuroscience of suicidal ideation demonstrates that social connection reduces stress hormone levels, decreases inflammation, increases oxytocin and other bonding chemicals, and activates reward circuits in the brain. When people feel genuinely connected to others, their HPA axis stress response normalizes, their serotonin systems function better, and their prefrontal cortex maintains better regulatory control.
Conversely, social isolation has effects on the brain comparable to significant risk factors like smoking. The neuroscience of suicidal ideation shows that loneliness activates inflammatory pathways, dysregulates stress systems, and impairs the prefrontal cortex’s ability to regulate emotions. Connection isn’t a luxury; it’s a biological necessity for brain health.
Movement as Brain Medicine
Physical activity represents another intervention strongly supported by the neuroscience of suicidal ideation. Exercise increases BDNF production, promotes neuroplasticity, reduces inflammation, improves sleep quality, regulates stress hormones, and activates reward circuits. Studies indicate that people who engage in regular physical activity report nearly 50 percent lower levels of suicidal thoughts.
The neuroscience of suicidal ideation reveals that exercise works through multiple pathways simultaneously. It improves sleep, which is critical because sleep disturbances independently predict suicidal thoughts and behaviors. It reduces depressive symptoms by restoring neurotransmitter balance and promoting neuroplasticity. It provides a sense of mastery and self-efficacy that counters hopelessness. Exercise in natural settings amplifies the benefits even further.
The neuroscience of suicidal ideation reveals that even moderate exercise can yield significant benefits. Even moderate activities like walking can produce meaningful changes in brain chemistry and structure. The key is consistency; regular activity creates sustained changes in neural functioning that build resilience over time.
The Role of Sleep in Brain Recovery
Sleep consistently appears in the neuroscience of suicidal ideation as a risk factor when disturbed and a restorative mechanism when optimized. Sleep disturbances independently predict suicidal thoughts and behaviors, even in otherwise healthy individuals. The neuroscience of suicidal ideation shows that during sleep, the brain clears metabolic waste products, consolidates emotional memories in healthier ways, restores neurotransmitter balance, and repairs neural connections.
Poor sleep quality increases suicide risk by reducing the ability to cope with stress, impairing prefrontal cortex functioning, intensifying emotional reactivity, and promoting inflammation. When someone is sleep deprived, all the brain mechanisms that protect against suicidal thinking become compromised. Conversely, significant reductions in suicide risk can result from improving sleep quality through sleep hygiene practices, addressing sleep disorders, and establishing regular sleep-wake cycles.
Hope as a Neurobiological State
The neuroscience of suicidal ideation has commenced an investigation into hope as a quantifiable brain state possessing protective attributes. Hope isn’t just wishful thinking; it involves specific cognitive patterns, future-oriented thinking, goal-directed behavior, and belief in one’s agency.
These mental processes engage prefrontal regions, activate reward circuits, and counter the hopelessness that characterizes suicidal states. Warning signs of suicidal ideation include persistent hopeless thoughts, social withdrawal, sleep disruption, loss of pleasure in activities, and increased talk about being a burden, all reflecting measurable brain changes addressable through neuroscience-based coaching.
Research shows that interventions specifically designed to build hope, meaning, and purpose produce measurable changes in brain activation patterns and significantly reduce suicide risk. The neuroscience of suicidal ideation demonstrates that when people develop a sense of meaning and purpose, their brain’s reward systems become more responsive, their prefrontal cortex maintains better regulatory control, and their stress response systems function more adaptively.
Finding meaning doesn’t require grand gestures or significant life changes. The neuroscience suggests that even simple practices like gratitude journaling, identifying personal values, setting small achievable goals, and connecting daily activities to larger purposes can shift brain functioning in protective directions. Each small step toward meaning creates neural changes that accumulate over time.
The Compassionate Path Forward
Understanding the neuroscience of suicidal ideation fundamentally changes how we view people in crisis. These aren’t weak individuals making selfish choices; they are people whose brains have been altered by trauma, stress, inflammation, chemical imbalances, and disrupted connectivity. Their suffering is real, their biology is compromised, and they deserve compassion, not judgment.
The neuroscience of suicidal ideation also offers genuine hope. Every mechanism that creates vulnerability represents a potential intervention point. Prefrontal cortex dysfunction can be addressed through therapy and skill building. Changes in lifestyle and medication can help correct neurotransmitter imbalances. Inflammation can be reduced through diet, exercise, and stress management. White matter disruptions may improve as stress decreases and health improves. Neuroplasticity means the brain can mend and rewire itself toward wellness.
If you’re struggling with suicidal thoughts, please know that what you’re experiencing reflects changes in your brain that can be reversed. The thoughts feel permanent, but the neuroscience of suicidal ideation proves they’re not. Your brain can mend, chemical balance can be restored, neural connections can be rebuilt, and hope can return. You are not your thoughts; you are a person whose brain is temporarily creating thoughts that don’t reflect reality or your future possibilities.
Reach out for help. Call a crisis line, tell someone you trust, see a mental health professional, or go to an emergency room. Every intervention, whether it’s connection, therapy, medication, or lifestyle changes, helps restore balance to your brain. The neuroscience of suicidal ideation shows us that restoration is possible, recovery is real, and the brain’s remarkable capacity for change means that hope is always justified. Your life has value, your suffering can decrease, and your future can be different from your present. The biology of despair can transform into the biology of hope, one intervention and one day at a time.
Frequently Asked Questions About Neuroscience-Based Coaching for Suicide Prevention
Why is your neuroscience-based approach considered a game changer in suicide prevention?
Most suicide prevention models focus on crisis hotlines or periodic therapy with limited continuity. What sets this practice apart is a neuroscience-based framework in which every strategy honors how the brain really works under stress and during crisis. This method is not about one-size-fits-all advice, it combines deep knowledge of neurobiology with highly personalized coaching designed to rewire the root mechanisms fueling suicidal ideation. The result is an approach that doesn’t just manage symptoms temporarily but creates measurable, lasting change in brain pathways, giving clients true hope for lifelong resilience.
Why does 24/7 direct access to you make such a significant difference for clients?
Crisis moments are unpredictable and don’t wait for an appointment slot. Traditional mental health services often require clients to wait days or even weeks for help, and emergency hotlines connect you to strangers unfamiliar with your history. With 24/7 access, you reach out directly to a doctor who knows your brain, tracks your patterns, understands your triggers, and is truly invested in your life. This ongoing relationship means support arrives exactly when and how you need it, dramatically increasing safety while giving the brain the real-time corrective experiences required for true neuroplastic change.
How does neuroplasticity training genuinely re-wire unhealthy thought patterns instead of just providing coping skills?
Neuroplasticity is the brain’s natural capacity to change and adapt by forming new neural connections. In our work together, you’ll do far more than “cope”—you’ll practice thought reframing, cognitive correction, and emotional regulation until these new strategies are automated by your brain. This “training” goes beyond talk, engaging techniques such as guided neural rehearsal and immediate real-life implementation during crisis via text, call, or message. Over time, the brain reinforces these healthier patterns so strongly that old, harmful defaults become less accessible, and positive, adaptive responses become your brain’s go-to mode.
What is “thought reframing,” and why is it so essential in neuroscience-based suicide prevention?
Thought reframing, as taught in this practice, is not just “positive thinking.” It is a neuroscience-backed process that empowers your rational brain to interrupt and observe the outputs of a dysregulated system—such as catastrophic or hopeless thoughts—without automatically believing them. By learning to identify and name the specific brain states behind each negative thought, you develop the ability to pause, redirect, and begin reshaping your thinking in real time, leveraging your brain’s own circuitry. This approach weakens dangerous thought loops and strengthens the neural networks supporting insight, calm, and hope.
How is working with you different from calling a suicide hotline or seeing a therapist just once a week?
The major difference is relationship, real-time access, and precision neuroscience. With you, support comes from a professional who knows your history, watches for your personal warning signs, and can intervene before a full-blown crisis. Unlike a hotline where the person on the other end is a stranger, and unlike weekly therapy that may not cover urgent needs, this practice provides a steady partnership and the correct neurobiological interventions as often as needed. Over time, this builds a foundation of trust, promotes faster brain recovery during stress, and enables permanent, life-affirming change, redefining what’s possible in suicide prevention.