🎧 Audio Version
When I talk about the neuroscience of rumination with high achievers, they almost always say the same thing. They know they are overthinking, they know it makes everything feel heavier, and yet their brain will not let go. The mind replays the same meeting, the same argument, and the same fear, as if grinding on it harder will finally change the outcome.
For more than twenty-five years, I have studied what happens in the brain when it gets stuck in these loops. Inside MindLAB Neuroscience, I work with executives, founders, and professionals who live with PTSD, depression, anxiety, and ADHD. For them, the neuroscience of rumination is not theory. It is the difference between falling asleep in ten minutes or staring at the ceiling at three in the morning with a heart that will not slow down.
In this article I will walk you through the neuroscience of rumination in simple, human language. You will see which brain networks are involved, why some brains are more vulnerable, how repetitive thinking shows up in PTSD, depression, anxiety, and ADHD, and what you can actually do to retrain your nervous system. My goal is to help you move from harsh mental replay to grounded reflection that serves your life instead of draining it.

What Is Rumination: The Neuroscience of Rumination in Simple Terms
Before we go deeper into the neuroscience of rumination, we need a clear definition. Rumination is not just thinking a lot. Stewing is repetitive, sticky thinking that circles around what is wrong, what went wrong, or what might go wrong, without moving you toward a real solution.
Healthy reflection might sound like this. That meeting did not go how I wanted. What can I learn, and what will I try next time? The energy is curious and forward moving. Rumination sounds very different. Why did I say that? They probably think I am useless. I always mess things up. The energy is tight, self-attacking, and endless. The neuroscience of rumination helps explain why the first style of thinking is flexible, while the second style becomes a mental cage.
Psychological rumination is the habit of turning the same painful thoughts over and over in your mind without gaining relief, insight, or a real plan
Rumination is usually past-focused. You replay an argument from last week. You relive a mistake from years ago. You mentally confront someone who hurt you or humiliate yourself in your own mind over and over. Worry is more about the future, but the same brain circuits often drive both, which is why the neuroscience of rumination overlaps with the neuroscience of anxiety.
Rumination is also passive. You are not calmly solving a problem. You are spinning inside the problem. You feel compelled to think about it, but you do not feel more prepared. You feel more stuck. At the brain level, rumination tricks your nervous system. It feels like you are working, but you are really reinforcing the same painful pathways.
The Neuroscience of Rumination in Key Brain Networks
When I teach clients about the neuroscience of rumination, I use a simple model. Your brain is not one thing. It is a group of networks that can either cooperate or compete. Rumination happens when certain networks overpower others, especially under stress.
One of the main networks in the neuroscience of rumination is called the default mode network. It includes areas like the medial prefrontal cortex and the posterior cingulate cortex. This network lights up when you are not focused on a task. It supports daydreaming, mental time travel, and your inner story about who you are.
In a balanced brain, the default mode network shares control with task-focused networks that help you plan, focus, and act. In a ruminating brain, the default mode network becomes overactive and biased toward negative, self-critical stories. If you have depression, this can sound like a constant inner narrator listing your flaws. If you have anxiety, it creates detailed disaster scenarios. The neuroscience of rumination shows that this network keeps pulling you back into replay mode whenever your mind has space.
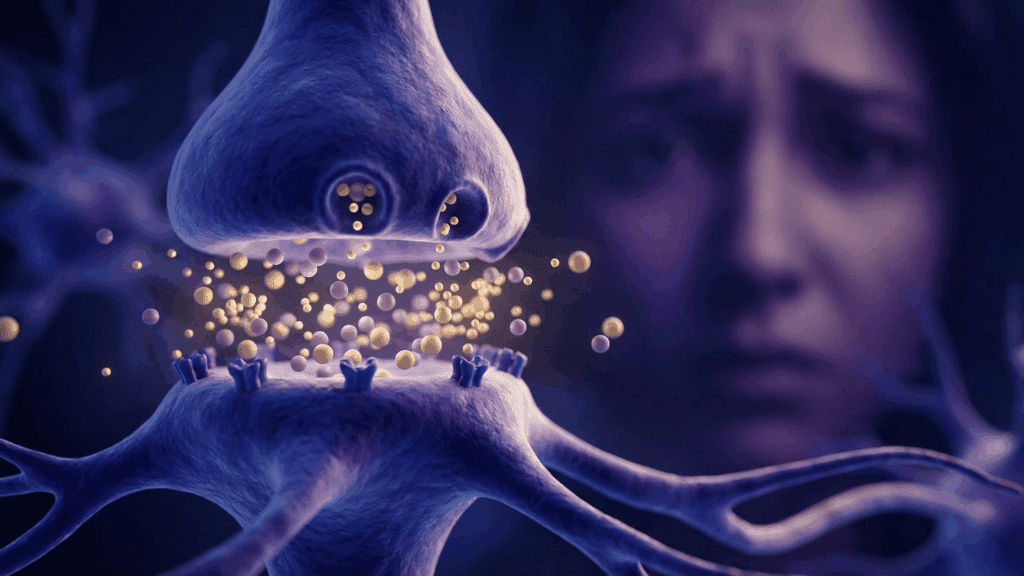
Another key player is the amygdala, the brain’s alarm system. It sits deep in the temporal lobe and scans for threats. When you live with PTSD, chronic stress, or long-term criticism, the amygdala learns to fire more quickly and more often. Small cues, like a tone of voice or a slight pause in an email, can trigger a full survival response.
Once the amygdala sends an alarm, your brain begins searching for danger. In rumination, that danger is often inside your own head. You scan your past for where you messed up. You imagine how others might judge you. You replay painful scenes. The neuroscience of rumination shows that the amygdala and the default mode network talk to each other. The more the amygdala fires, the more the default mode network spins up negative stories. Those stories keep the amygdala on edge, and the loop feeds itself.
The prefrontal cortex, especially the areas right behind your forehead, is supposed to act like a wise coach. It helps you regulate emotion, hold perspective, and choose what to focus on. In PTSD, depression, anxiety, and ADHD, this coach can become worn out, underactive, or overwhelmed.
When the prefrontal cortex is offline, the alarm systems and the default mode network run the show. You might know you are spiraling, yet still feel unable to shift. The neuroscience of rumination explains that in those moments your regulatory circuits simply do not have enough strength to calm the alarm and redirect your focus. You are not weak. Your brain is firing in a pattern it has rehearsed for years.

How Neurochemistry Fuels the Neuroscience of Rumination
The neuroscience of rumination is not only about where activity happens in the brain. It is also about the chemistry that carries signals between cells. Neurotransmitters and hormones shape your mood, attention, and flexibility.
Serotonin is one major player. It supports mood regulation and cognitive flexibility, which means your ability to shift your thinking. When serotonin signaling is low or disrupted, it becomes harder for the brain to change gears. Many clients with depression tell me that their thoughts feel heavy and slow, yet also hard to escape. The neuroscience of rumination shows that when serotonin is not doing its job well, negative thoughts have an easier time sticking.
Dopamine brings another layer. People often think of dopamine only as the reward chemical. In my work on dopamine and motivation, I often explain that dopamine is about attention, drive, and what your brain decides is important. If your brain has learned that analyzing every mistake might protect you from future pain, it can give you a small dopamine hit when you start to ruminate. It feels like you are doing something productive, even when you are only drilling into the same wound.
This is why the neuroscience of rumination treats it like a habit. Your brain learns that going over the same story creates a sense of control. That false sense of control becomes reinforcing. Dopamine says, Keep going; you might finally figure it out. The truth is that you are only deepening the groove.
Cortisol, the main stress hormone, also shapes the neuroscience of rumination. Chronic stress keeps cortisol elevated. High cortisol makes your amygdala more reactive. It dulls the prefrontal cortex and wears on the hippocampus, the brain’s memory librarian. When someone with PTSD tells me that a ten-year-old event feels like it happened last week, I see cortisol’s footprint. The nervous system is still on alert, ready to replay and relive the past.
When you put all of this together, the neuroscience of rumination shows a clear pattern. The alarm system is jumpy, the self-focused network is biased toward negative stories, the wise coach is tired, and the chemistry that should support flexibility is out of tune. That is a perfect recipe for getting stuck.
Why Certain Brains Are Prone to the Neuroscience of Rumination
Not every brain ruminates in the same way or to the same degree. The neuroscience of rumination helps explain why some people can let things go while others feel haunted for days.
Part of this comes from temperament. Many of my clients are sensitive, perfectionistic, and highly conscientious. Their brains are excellent at picking up patterns and small errors. That skill can be a gift in leadership and high-level work. Without self-compassion, it becomes fuel for rumination. The mind turns that sharp lens inward. The neuroscience of rumination shows that a highly observant brain, combined with a harsh inner voice, is a prime target for loops.
History also plays a large role. If you grew up in a home where love felt conditional, where mistakes were punished, or where emotions were dismissed, your nervous system learned that constant self-monitoring might keep you safe. I see this in many clients with depression and anxiety who describe an inner critic that sounds suspiciously like an old parent, teacher, or coach.
For clients with PTSD, the neuroscience of rumination sits right on top of survival wiring. The brain becomes consumed with preventing the trauma from happening again. It replays every detail, every choice, every angle, trying to find the moment when things could have gone differently. This search is not logical. It is an expression of a nervous system desperate to feel safe.
In ADHD, the picture is different but related. ADHD brains are often fast, creative, and full of ideas. At the same time, repeated experiences of being late, missing details, or getting criticized can create deep shame. Many of my ADHD clients say their mind bounces from one self-critical thought to another. They replay missed deadlines and awkward interactions long after everyone else has moved on. Their fast brain makes the rumination even more intense.
Current lifestyle also shapes the neuroscience of rumination. Poor sleep, constant digital stimulation, and a lack of real restorative time keep the nervous system in a state of mild threat. A tired, overloaded brain has less capacity to regulate itself. When you finally stop working and look at your phone in bed, your default mode network grabs the chance to drag you back into old stories.

How the Neuroscience of Rumination Shows Up in PTSD, Depression, Anxiety, and ADHD
Because I work at the intersection of neuroscience and coaching, I see the neuroscience of rumination express itself differently in PTSD, depression, anxiety, and ADHD. The underlying circuitry overlaps, but the stories your brain tells are not the same.
In PTSD, rumination is often about survival. A former client, I will call her Maria, survived a serious car accident. Months later she was physically safe, but her brain did not accept that. Any time she tried to drive, her mind replayed the sound of the crash, the smell of burned rubber, and the feeling of her chest crushing against the seat belt. At night she lay awake reviewing every decision she made on the day of the accident.
In Maria’s brain, the amygdala was hypersensitive, and the default mode network was saturated with fear memories. The neuroscience of rumination helped her see that her brain was not trying to torture her. It was trying, in a misguided way, to protect her from another crash by never letting her forget the first one.
In depression, rumination often sounds like a cruel narrator living inside your head. Rumination and depression feed into each other, because the more your mind loops on old mistakes, the heavier and more hopeless your mood can feel. Another client, I will call him James, was a successful executive who could not understand why life felt so flat and heavy. He told me he spent hours each week mentally listing his failures and shortcomings. A small setback at work would trigger thoughts like, I am a fraud; nothing I do matters.
For James, the default mode network had become overactive and locked onto shame-based stories. The serotonin system that should support flexible thinking was struggling. The prefrontal cortex had trouble stepping in with a balanced view. The neuroscience of rumination helped him see that these thoughts were not objective truth. They were a tired pattern his brain had rehearsed for years.
In anxiety, rumination spends more time in the future. A client I will call Leila had intense social anxiety. For days before a presentation, she played out every possible disaster. She imagined forgetting her words, seeing her boss roll his eyes, and feeling her face flush bright red. After meetings she replayed every remark she had made, searching for evidence that her colleagues thought she was incompetent.
In her case, the amygdala treated almost every social interaction as a threat. The default mode network used those alarms to write detailed worst-case scripts. The neuroscience of rumination made it clear that her brain had learned to equate visibility with danger.
In ADHD, rumination often mixes with time blindness and rejection sensitivity. A client I will call Rob had a long history of missed deadlines and forgotten tasks. Each time something slipped, he would mentally beat himself up for days. He imagined his boss planning to fire him. He replayed old report cards where teachers called him lazy. His quick brain moved from memory to memory so fast that his body felt wired and drained at the same time.
Rob’s dopamine system chased quick hits of distraction to get away from painful thoughts, while his default mode network chewed on memories of failure. The neuroscience of rumination helped him see that his brain was not broken. It had simply learned a painful pattern that could be replaced.

The Hidden Costs and Daily Impact of the Neuroscience of Rumination
When clients come to MindLAB Neuroscience, they often name PTSD, depression, anxiety, or ADHD as their main concern. As we unpack their story, I almost always find that the neuroscience of rumination is quietly making everything worse.
On a mental level, rumination pulls your mood down. Over time, this kind of negative brooding quietly reshapes how you see yourself, your relationships, and the future you believe is possible. If your inner world is filled with criticism, regret, and rehearsals of fear, your brain continues to strengthen the pathways that reinforce those negative states. Over time you start to believe that your current state is simply who you are. In reality, you are repeatedly firing the same circuit. Neuroplasticity means your brain will get better at whatever you practice, including tearing yourself apart.
On a thinking level, rumination steals your bandwidth. Old arguments, imagined disasters, and self-blame can occupy half your attention, leaving less room for creativity, planning, and deep work. Many executives tell me they feel foggy or distracted. When we trace it, we find that a huge portion of their day is spent in silent, invisible mental battles.
On a physical level, the neuroscience of rumination keeps your stress response on a low simmer. The body responds to vivid imagination almost as strongly as to real events. When you relive a betrayal or humiliation, your heart rate, blood pressure, and muscle tension shift as if it is happening again. Over time this takes a toll on your cardiovascular system, your immune system, and your sleep quality.
Relationships also absorb the impact of this overthinking pattern. When your mind is stuck on replay, it is hard to be present with the people you love. You might take an offhand comment from your partner and turn it into a story about rejection. You might obsess over a text that came without an emoji and turn it into proof that a friend is angry. This condition is even more intense when PTSD or anxiety is involved, because the brain is already primed to look for danger.
Perhaps the deepest cost of the neuroscience of rumination is how it narrows your sense of possibility. When your inner world is filled with old pain and imagined catastrophe, it becomes very hard to picture a different future. The same neuroplasticity that could help you change is hijacked to keep you stuck.

Rewiring the Neuroscience of Rumination with Brain-Based Strategies
The encouraging news is that the neuroscience of rumination also offers a path out. Because obsessing is a learned brain pattern, it can be unlearned. This is not about forcing positive thoughts. It is about training new neural pathways that slowly become your default.
The first step is awareness without attack. When a client says, “I am doing it again; I am stuck in my head,” I ask them to pause and notice where they feel it in the body. Do they feel a knot in the stomach, a tight jaw, or a buzzing in the chest? Bringing gentle attention to the body begins to move activity from the amygdala into the prefrontal cortex. The wise coach starts to wake up.
The second step is attention training. If your brain has spent years going wherever it wants, your attention muscles are weak. We start very small. For example, placing one hand on the abdomen and feeling ten slow breaths. Or listening for sounds in the room for sixty seconds without chasing thoughts. Each time the mind drifts back into mental replay, you simply and kindly return to the chosen focus.
From a neuroscience perspective, this is like doing repetitions at the gym for your prefrontal cortex. Over time, these simple practices change the neuroscience of rumination. The regulatory circuits grow stronger and better able to quiet the default mode network when it starts to spin.
The third step is learning a new way to talk to yourself. Many people with depression and anxiety have inner voices that are brutal. Instead of jumping to fake positivity, we aim for realistic, kind statements. For instance, That call did not go the way I wanted, but it is one call in a long career, and I know specific things I can adjust next time. When you practice this style of thinking over and over, the default mode network receives new stories to rehearse. The amygdala has fewer reasons to sound the alarm.
The fourth step is returning to the body on purpose. A thought loop lives in the head, but regulation lives in the entire nervous system. I often teach paced breathing, gentle movement, or sensory grounding, such as feeling your feet on the floor or holding something cool. These practices send calming signals through the vagus nerve. They tell your survival brain that right now, in this moment, you are safe enough.
In PTSD, depression, anxiety, and ADHD, the specifics of these steps vary. The map from the neuroscience of rumination helps me design routines that fit each unique brain. A protocol that works for a perfectionistic executive with depression will look different than a protocol for a founder with ADHD and rejection sensitivity. The principles remain the same. Rewire attention, update your inner story, and calm the body so that the higher brain can come back online.

A MindLAB Neuroscience Framework for Transforming Rumination
Over more than twenty-five years, I have turned these ideas into a clear framework inside MindLAB Neuroscience that directly targets the neuroscience of rumination.
We begin with education. When clients understand the repetitive thinking, they stop seeing themselves as defective. They begin to see their rumination as a pattern that once served a purpose, usually protection, but is now outdated. This shift reduces shame, and a brain with less shame is more able to change.
Next we map their personal version of this pattern. When does circular thinking show up the most? What are the first thoughts that signal a loop? How does it feel in the body? How do PTSD, depression, anxiety, or ADHD color the stories that play? No two maps are the same, because no two lives are the same.
Then we build daily practices that gently reshape the neuroscience of rumination. For one client with PTSD, that might mean a short grounding routine before and after driving, plus an evening reflection that focuses on resilience instead of replaying the trauma. For a client with depression, it might involve a morning body check-in, scheduled blocks for focused work to keep the default mode network in balance, and a nightly review of three small wins to nudge the brain toward a more accurate story.
We also look closely at relationships. The neuroscience of rumination does not operate in isolation. If your partner shuts down when you speak up, your brain will tell one kind of story. If your team at work is chaotic and critical, your loops will look different than if you are surrounded by supportive, emotionally aware colleagues. In coaching, we explore how to communicate your inner experience so that you are not fighting this battle alone.
Finally, we keep a steady focus on hope grounded in neuroplasticity. I have watched clients who spent decades trapped in mental looping move into lives that feel spacious and connected. PTSD symptoms soften. Depressive episodes become less frequent and less intense. Anxiety becomes something they can understand and manage instead of a mysterious wave that swallows them. ADHD brains that once used their speed only for self-attack learn to use that speed for creativity and problem-solving.
The neuroscience of rumination explains why your brain gets stuck. It also shows that your brain is not fixed in that state. With the right understanding, consistent brain-based practices, and the support of a neuroscience-informed guide, you can teach your mind to return to the present, to reflect instead of relive, and to build a future that is not ruled by old loops.
Frequently Asked Questions About the Neuroscience of Rumination
What exactly is rumination from a neuroscience point of view?
Worry loops involve more than simply thinking a lot. From a neuroscience perspective, rumination is a repetitive thought loop that keeps the brain locked on what is wrong, what went wrong, or what might go wrong, without moving into real problem solving. The default mode network, which creates your inner story and mental time travel, becomes overactive and biased toward negative narratives. The amygdala, your internal alarm system, keeps scanning for threats, and the prefrontal cortex, which should guide and regulate, struggles to step in. When these systems fall out of balance, the neuroscience of rumination shows up as a mental echo chamber that feels compelling but does not actually help you move forward.
Why does my brain ruminate more when I have PTSD, depression, anxiety, or ADHD?
In PTSD, the brain is trying to protect you from danger. The amygdala fires quickly, and the default mode network replays the trauma to search for ways you could have prevented it. The neuroscience of rumination here is driven by survival wiring that has not turned off. In depression, the default mode network is often stuck on self-critical stories like I am a failure, nothing will change. Low mood and low energy make it harder for the prefrontal cortex to offer a more balanced view, so the loop keeps spinning. With anxiety, the brain uses repetitive thinking to run through endless worst-case scenarios. The amygdala treats uncertainty as a threat, and the mind rehearses disasters in an attempt to feel prepared. In ADHD, a fast, creative brain mixed with years of criticism can turn into rapid-fire rumination about mistakes, missed deadlines, and perceived rejection. Dopamine-driven attention jumps from one self-attacking thought to another. The neuroscience of rumination explains why all four conditions can make it harder to shift attention and let go.
Is rumination ever helpful, or is it always a problem?
Short, focused reflection can be very helpful. When you calmly review an event, look for lessons, and decide what to try next, your prefrontal cortex is in charge and your emotional brain is regulated. That is healthy learning. The neuroscience of rumination becomes relevant when the thinking no longer leads to insight or action. If you keep replaying the same moment and feel worse, if your body is tight and your mind is harsh, your brain is not problem-solving. It is rehearsing pain. Over time, this repetition strengthens the neural circuits associated with anxiety, depression, PTSD symptoms, and feelings of shame. This is a simple test. After ten minutes of thinking about the situation, do you feel clearer and more grounded, or more flooded and stuck? If you feel flooded, your brain has probably crossed from reflection into brooding.
Is it possible for me to retrain my brain to move away from rumination, or is this simply part of my natural wiring?
You are not stuck with the neuroscience of rumination for life. Neuroplasticity means your brain can change its structure and function when you repeatedly practice new patterns. I have watched clients who spent decades in constant rumination learn to shift their focus, quiet their inner critic, and feel safe enough to be present. This change does not happen overnight, but it is absolutely possible. When you use body-based grounding, attention training, and realistic self-talk, you are building new pathways in the prefrontal cortex and calming the amygdala. When you gently interrupt dwelling and choose a different focus again and again, the default mode network starts to tell a different story. The neuroscience of rumination is not a life sentence. It is a map that shows you why your brain gets stuck and where you can apply specific, repeatable practices to move it toward flexibility and calm.
What is one practical first step to interrupt rumination when it shows up?
The first step is not to argue with the thoughts. That usually pulls you deeper into the loop. Instead, use a simple protocol that engages both brain and body. As soon as you notice the worry loop in action, name it gently. You might say to yourself, My brain is looping right now. Then shift attention into the body. Place a hand on your abdomen and feel ten slow, even breaths. Notice the rise and fall under your hand. If your mind drifts back to the story, kindly bring it back to the physical sensation. This tiny practice does three important things. It activates the prefrontal cortex through mindful attention, it sends calming signals through the nervous system, and it breaks the automatic link between a trigger and an old thought loop. Over time, repeating this simple step begins to rewire the neuroscience of rumination into a pattern that includes awareness, grounding, and choice.